Gastric sleeve surgery explained
- Overview
When it comes to bariatric surgery, one size doesn’t necessarily fit all. That’s why there are plenty of options to suit your needs. Most patients look for a permanent change with a high rate of success. For people in this position, two options stand out: gastric bypass and sleeve gastrectomy.
Bypass vs sleeve
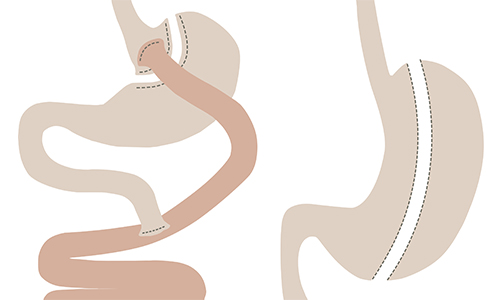
While gastric bypass still has the highest rates of success, it is a more complex procedure requiring two joins in the stomach. The nature of the operation also means patients experience absorption issues and need to take supplements for the rest of their lives to make sure they absorb enough nutrients.
Sleeve gastrectomy gets around these issues by stapling off a portion of the stomach and removing the excess – effectively turning it from a pouch into a sleeve. As no part of the stomach is bypassed, nutrients are absorbed in the usual way. However, the restrictions on the amount of food patients are able to eat means they will still need to take supplements. The results are excellent, achieving up to 70 percent excess weight loss, just shy of the standard set by the gastric bypass. Nonetheless, it is a simpler solution, both in the operation and the way the patient’s life is affected afterwards.
Added benefits
As well as weight loss, sleeve gastrectomy has also been proven to bring about remission of diabetes. In some cases the need for diabetic medication is eliminated within hours of the surgery being completed.
See how sleeve gastrectomy changed Alison’s life.
Who can have a sleeve gastrectomy?
The current guidelines recommend bariatric surgery as an option for people with a BMI over 35 with comorbidities (obesity-related illnesses such as diabetes) or people with a BMI over 40 with or without comorbidities.
Surgery alone doesn’t lead to successful weight loss. It requires the help of a multi-disciplinary team and the engagement of the patient.
Read 3 hard truths about weight loss surgery.
What’s involved in gastric sleeve surgery?
The patient journey involves meeting with a surgeon and a dietician before the operation. Patients have to make significant changes to their diet and lifestyle even before the operation to get in shape for the procedure and prove they have the discipline to stay on track afterwards.
The operation itself is usually completed within three hours. The patient will be put under general anaesthetic while the procedure is carried out laparoscopically (through an instrument inserted into the abdomen via keyhole surgery).
After the operation the way they will be able to eat and how much they will be able to eat changes significantly. It can be a difficult process requiring help and support from the dietician team as well as ongoing help and advice from surgeons. It’s certainly not an easy fix but it can be a life-changing and even life-saving procedure.
Interested in gastric sleeve surgery?
Fill in the form below and we'll get back to you within one working day.
Thank you
A member of the team will respond to you soon.
Last updated Wednesday 26 February 2020
First published on Monday 22 February 2016



