Knee replacement (Total knee replacement)
- Overview
Or call us on
Knee replacement, or total knee replacement, is a surgical procedure to remove the damaged knee joint and replace it with an artificial joint.
What is a knee replacement?
Knee replacement, also known as total knee replacement or knee arthroplasty, is a surgical procedure that removes and replaces the damaged knee joint with an artificial joint. The most common reason you need a knee replacement is because of damage to your knee caused by knee osteoarthritis, which is the gradual wear and tear of the joint.
During the procedure, both sides of the damaged joint are removed and replaced with an implant. If your arthritis is minimal, you may be able to have a partial knee replacement.
What is knee osteoarthritis, and what are other causes of chronic knee pain?
The most common causes of long-term (chronic) knee pain that may need a knee replacement are:
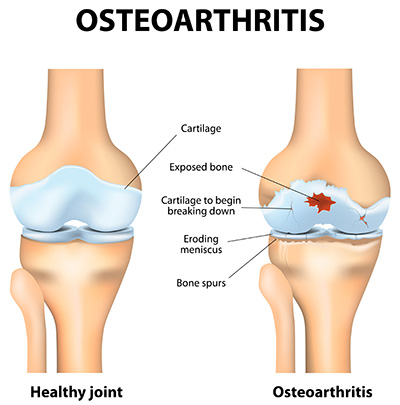
- Osteoarthritis is a degenerative joint disease where the protective cartilage that cushions the ends of your bones wears down over time. It is often called "wear and tear" arthritis and is common in older adults, but it can also affect younger people. Symptoms include knee pain, stiffness, swelling and reduced movement.
- Rheumatoid arthritis is an autoimmune disease where the body's immune system attacks the lining of the joints (synovium), causing inflammation, pain, swelling, and eventually, erosion of cartilage and bone.
- Post-traumatic arthritis: This can develop after a knee injury, such as a fracture, ligament tear, or meniscus injury, which damages the cartilage and leads to premature wear.
Other conditions, such as gout or avascular necrosis, can also lead to significant damage to the knee joint, potentially requiring replacement.
Types of knee replacement:
- Total knee replacement: All three compartments of the knee (medial, lateral and patellofemoral) are replaced.
- Partial knee replacement: Only one compartment of the knee is replaced.
- Kneecap replacement: Involves replacing the underside of the kneecap and the groove it sits in. This is also known as patellofemoral arthroplasty.
- Revision knee replacement: Replaces a previous knee replacement that has failed or worn out.
Is a knee replacement right for me?
Your consultant may recommend a knee replacement if:
- You experience severe knee pain that affects everyday activities like walking, climbing stairs or getting in and out of chairs.
- Your knee pain persists even while resting or sleeping.
- You experience knee swelling and inflammation that doesn't improve with rest or medication.
- You’ve tried alternative treatments, such as physiotherapy, pain relief, walking aids or joint injections, and they haven’t helped.
While most people who have a knee replacement are between 60 and 80 years old, with the average age at 69, many younger patients also benefit from surgery when other treatments haven't helped.
The decision to have a knee replacement is made jointly by you, your GP, and your surgeon. There is almost never an absolute indication for knee replacement surgery, but ultimately, the decision is yours.
What are the benefits of a knee replacement?
A knee replacement can offer many helpful benefits, especially for people with severe joint damage or arthritis:
- Pain relief: the most common and significant benefit. Replacing the damaged knee joint helps to reduce or stop chronic knee pain that limits daily life.
- Improved mobility and function: Many people find walking, climbing stairs, and carrying out everyday activities easier after surgery.
- Enhanced quality of life: You can return to what you love doing and enjoy greater independence.
How long do the benefits last?
For most people, knee replacements typically last 15 to 20 years, and some can last even longer. Staying active, maintaining a healthy weight and following your doctor's advice can help your new knee last longer. After that time, you may need a knee replacement revision follow-up surgery to replace or repair the artificial joint.
What happens during a knee replacement?
What happens before knee replacement?
You will meet with an orthopaedic surgeon who will review your medical history and examine your knee, assessing its range of motion, stability and strength. They will also review your X-rays or other imaging results. During the consultation, your surgeon will explain the possible risks and benefits of knee surgery, discuss the different surgical techniques, and recommend the best option for you.
Feel free to speak with your surgeon about any concerns or questions about the surgery or your recovery. They are here to help you feel informed and confident.
Preparing for surgery
Your surgeon and the hospital team will give you instructions on preparing
for surgery, and it is important to follow them carefully.
- Let your doctor know about any medication you take. They will let you know if you should continue or temporarily stop any medicines before and after your surgery.
- If you smoke, stop smoking several weeks before the operation.
- Try to maintain a healthy weight.
- Exercise regularly.
- Don’t shave or wax the area where a cut will likely be made.
- Try to have a bath or shower the day before or on the day of the operation.
- Prepare your home for your post-surgery recovery. Remove trip hazards and place essential items within easy reach.
- Arrange transportation: You won't be able to drive after surgery, so make sure someone can pick you up from the hospital and take you home. You'll also need help around the house during the first few weeks of your recovery.
During the surgery
Knee replacement surgery is usually performed under spinal or general anaesthesia, sometimes combined with a local nerve block for added pain relief. You, the anaesthetist, and your surgeon will decide on the type of anaesthesia to be used.
To minimise the risk of infection, you’ll be given antibiotics in the operating theatre just before the start of surgery and for two or three doses afterwards, depending on the type of drug used.
The duration of knee replacement surgery can vary depending on the surgical technique, but it typically takes 1 to 2 hours.
There are different methods used for knee replacement surgery, depending on how badly the joint is damaged:
Traditional total knee replacement
- Once you’re under anaesthetic, your surgeon will cut the front of your knee.
- Damaged cartilage and bone are removed from the thigh bone (femur) and shin bone (tibia).
- The ends of the femur and tibia are carefully shaped to create new surfaces for the implant.
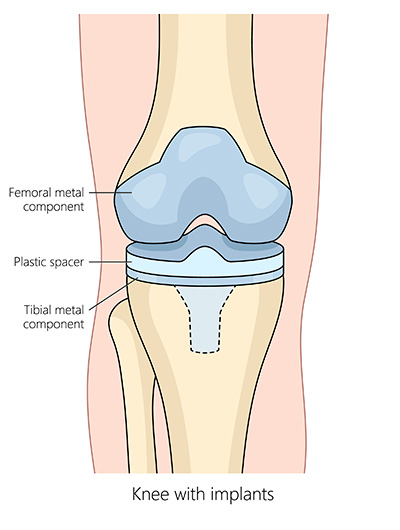
- The artificial implant is fitted over the ends of both bones, and a plastic spacer is inserted between them to create a smooth, gliding surface.
- The back of the kneecap (patella) may also be replaced with a plastic (polyethene) implant.
- The implant is fixed to the bones using an acrylic cement or a special coating that allows the artificial joint to bond directly to the bone over time.
- Finally, the cut is closed with stitches or surgical clips, and a padded dressing is applied. The dressing is removed after about 48 hours.
Robotic-assisted knee replacement
Robotic-assisted knee replacement uses advanced technology to help your surgeon work more accurately. This method can lead to faster recovery, shorter hospital stays, and better results for many patients.
At Nuffield Health, we use Stryker's Mako® Robotic-Arm Assisted Surgery System and CORI® Robotic-Assisted Surgical System for our robotic-assisted knee replacements.
Mako® Robotic-Arm assisted surgery
- Before your surgery, you will have a CT scan of your knee to create a 3D model of your knee joint. The 3D model is loaded into the Mako® system software to create a personalised surgical plan, which your surgeon will use during your surgery. The plan includes the implant's exact size, placement, and alignment.
- Your surgeon will cut the front of the knee to access the joint.
- Your surgeon will use the Mako® robotic arm to remove the damaged cartilage and bone from the thigh bone (femur) and shin bone (tibia).
- The artificial joint is implanted. The robotic arm guides your surgeon to stay within the pre-planned boundaries set by the 3D model, allowing for accurate implant positioning.
- The implant is fixed to the bones using an acrylic cement or a special coating that allows the artificial joint to bond directly to the bone over time.
- Your surgeon will check the new joint's stability, alignment, and movement before closing the cut with stitches or surgical clips and applying a padded dressing.
Find out more about Mako® Robotic-arm assisted total knee replacement.
CORI® Surgical System
- Your surgeon will use the CORI® system in the operating room to create a real-time 3D model of your knee. The 3D model is then used to create a personalised surgical plan, including the implant's exact size, placement, and alignment.
- Your surgeon will cut the front of the knee to access the joint.
- Your surgeon will use the handheld robotic-assisted tool to remove the damaged cartilage and bone from the thigh bone (femur) and shin bone (tibia). The CORI® system provides real-time feedback throughout the operation, helping your surgeon work more accurately.
- The artificial joint is implanted. The robotic-assisted tool helps your surgeon to position the implant accurately, allowing for a better fit and alignment.
- The implant is fixed to the bones using an acrylic cement or a special coating that allows the artificial joint to bond directly to the bone over time.
- Your surgeon will check the new joint's stability, alignment, and movement before closing the cut with stitches or surgical clips and applying a padded dressing.
Who is robotic-assisted knee replacement surgery suitable for?
Robotic-assisted knee replacement surgery may not be appropriate for all patients. Your consultant will advise you on the best treatments for your condition.
After the surgery
Once your knee replacement surgery is complete, you will be taken to the recovery room where a nurse will monitor you as you wake up. You may have a small tube in place to drain away any excess fluid from the surgical site and a drip (intravenous infusion) in your arm to keep you hydrated and provide pain relief medication.
The nurse will regularly check your wound, blood pressure and pulse. When you're fully awake and stable, you'll be taken to your hospital room.
You may need to stay in the hospital for 1 to 3 days, depending on how well you recover. You’ll be able to go home once your pain is managed, you can move around safely, and any necessary care or support has been arranged.
You'll be encouraged to stand and walk as soon as possible. A physiotherapist will help you with exercises to improve your knee's range of motion, build strength and safely manage stairs.
Recovery from knee replacement
Your wound is likely to take 10-14 days to heal. It may take up to 6 weeks to recover from the operation. It can take up to 12 months before you are back to normal activities.
Before you leave the hospital, your surgeon and healthcare team will give you instructions on recovering at home.
Short-term recovery
You may have help with the circulation in your legs through:
- Wear boots that are inflated with air for the first 2 days.
- Wear support stockings, which you should leave on for 4 to 6 weeks.
- Daily injections or tablets, which you may have for up to 6 weeks.
- Taking blood-thinning medication.
Walking around after a knee replacement
To help make your recovery go as smoothly as possible, you will need to start getting active and mobile as soon as you are able. We understand you may be nervous about getting up for the first time, but we’ll be there to help you whenever you’re ready. Getting mobile is all about confidence, which is why we help you progress through a range of walking aids until you’re independent.
- Day of surgery: A physiotherapist will give you some exercises to do while you’re in bed to help your new knee joint move and strengthen the muscles around it. Then they’ll help you get out of bed and start taking your first steps with a frame to prevent stiffness and maintain a healthy circulation.
- The day after surgery, you’ll have an X-ray to check the position of your new knee and some routine blood tests. If you haven’t started walking around yet, the physiotherapist will help you with this. Otherwise, you’ll continue practising walking using a frame with your nurse until you can do so on your own.
- Second and third day after surgery: An occupational therapist will give you tips for washing, dressing, and getting on and off the bed, chair, and toilet. The physiotherapist will help you transfer to crutches or a walking stick before giving you some more exercises to increase your movement.
Going home after knee replacement surgery
You’ll be able to leave as soon as you can safely walk up and down stairs on crutches, and the healthcare team is happy you are medically fit. However, you won’t be able to drive, so you’ll need someone to pick you up from the hospital and take you home.
We’ll train you to manage stairs in the following way:
- Use a handrail where possible with a walking aid in the opposite hand.
- If going downstairs, move the crutch or stick onto the lower step, put your weight on the crutch or stick as you move your operated leg onto the step alongside it.
- Bring your non-operated leg onto the same step and repeat.
- Do the opposite on the way back up..
Find out more about getting out of the car with crutches and getting into bed with crutches.
Managing your recovery at home
To begin with, it’s normal to experience:
- Tiredness – get plenty of rest, but it’s important to increase your activity slowly.
- Swelling –To ease your swelling, keep your leg raised when sitting and use the cryo cuff cold compress we gave you, or apply an ice pack wrapped in a tea towel.
- Pain – take any painkillers we’ve prescribed until you’re pain-free.
Here are a few things you can do to strengthen your knee, avoid damaging it and help your wound heal:
- Keep your wound dry for 4 to 5 days after your surgery, and use a waterproof dressing when you have a bath or shower.
- Continue the exercises the physiotherapist showed you.
- Try low-impact activities like walking, and gradually increase how far you walk.
- Keep using your crutches or walking stick for as long as you feel you need to.
- Don’t lift anything heavy or do any strenuous exercise.
- You can bend your knee 90-120 degrees, but you should avoid kneeling down.
- Don’t sit with your legs crossed for the first 6 weeks.
- Avoid twisting at your knee.
Call the healthcare team if you have any questions or concerns. If your calf becomes swollen, inflamed, or painful, seek medical advice as soon as possible.
Knee replacement recovery exercises
Initially, as you increase your activity, the knee can be sore, but with appropriate medication and gentle exercise, your recovery should proceed smoothly.
We’ll prescribe a set of exercises for you to do at home. Every programme is different, but here are a few exercises we regularly ask patients to do. You should aim for 3 sets of 10 reps per exercise every day:
- Stair lunges: Stand at the base of the stairs and place your operated foot on the first stair. Lunge forward, slowly bending at the knee only as far as is comfortable
- Bed exercise: Push the knee flat into the bed to fully straighten the leg
- Mini-squats: Stabilise yourself by holding on to a kitchen bench, door frame, or heavy table. Keep your back straight and lower your buttocks, bending at the knees. Only go as far as is comfortable.
Driving after a knee replacement
You should be able to start driving again after about 6 to 8 weeks, as long as you can operate the pedals and control your car in all situations. Any earlier than this and your reaction times may be too slow, particularly for emergency stops. Always check with your insurance company and your doctor first.
Time off work after a knee replacement
Taking time off to rest is essential, but returning to your routine as soon as possible can help you recover faster. If you have a desk job, you’ll be able to return to work after around 8 weeks. If your job is more physically demanding, you must wait around 12 weeks. If you’re not sure, check with your doctor.
Follow-up appointments
You’ll usually need to come back to have your stitches or staples removed about 2 weeks after your surgery, unless your surgeon used dissolvable stitches. Then, you’ll have a check-up with your consultant around 6 to 12 weeks after your surgery to make sure you’re recovering well. We’ll arrange these appointments with you before you leave the hospital.
It’s also recommended to have a check-up X-ray 12 months after surgery and monitor your implant.
Complications of a knee replacement
Most people recover well after knee replacement surgery, but like any other surgery, there may be complications. Your surgeon will discuss all the risks and complications of knee replacement surgery at your initial consultation.
General complications may include:
- Bleeding: Some bleeding is expected during and after surgery, but excessive bleeding should be reported to your consultant.
- Infection of the surgical site (wound).
- Allergic reaction to equipment materials and medication. Let your surgeon and healthcare team know if you have any allergies or have reacted to any medicine, test or dressings in the past.
- Blood clots (Deep vein Thrombosis DVT): A rare risk associated with any surgery.
Specific complications of knee replacement surgery:
- Nerve damage: Injury to the nerves around your knee, leading to weakness, numbness or pain in your leg or foot.
- Bone fracture: A crack or split in the bone may occur when the implant is inserted, especially if the bone is weak. Your surgeon may need to fix the fracture or use a different type of knee implant.
- Ligament or tendon damage: Ligaments or tendons near your knee can be damaged during surgery. Your surgeon may need to repair the damage using stitches, a piece of tendon from somewhere else in your body, or an artificial material.
- Infection: Infection around the implant can cause the knee replacement to loosen and fail. You will usually need one or more further procedures to treat the infection and restore joint function.
- Dislocation: Although rare in knee replacements, the artificial joint can become dislocated and may require correction or revision surgery.
- Persistent discomfort: Some patients may experience knee pain even if the knee implant replacement works well.
- Complex regional pain syndrome: A rare but serious complication involving chronic pain, stiffness and limited use of the knee after surgery.
Alternative treatment options to knee replacement surgery?
Ways to pay
Nuffield Health promise
Our prices are all-inclusive. We will equal any comparable price. There are no time limits on your aftercare.
Paying for yourself
There are no hidden costs in our treatment prices. The price you see is the price you pay.
Find out morePersonal medical loan
Spread the cost of your treatment with a 10, 12 or 24 month 0% personal medical loan.
Find out moreMedical insurance
We work with you and your insurance provider to get you the treatment you need quickly
Find out more