What is long COVID and how can it be treated?
- Overview
What is long COVID?
According to the NICE guidelines, the course of a COVID-19 illness can be split into the following phases:
- Acute COVID-19 – symptoms of COVID-19 that last for up to 4 weeks
- Ongoing symptomatic COVID-19 – symptoms of COVID-19 that last 4 to 12 weeks from the onset of the acute phase
- Post-COVID-19 syndrome – symptoms that develop during or after a COVID-19 infection, which continue for more than 12 weeks and aren’t explained by an alternative diagnosis.
‘Long COVID’ is commonly used for both ongoing symptomatic COVID-19 and post-COVID-19 syndrome.
Long COVID isn’t an illness that can be passed on to others like the acute COVID-19 infection – it’s a result of how your body has responded to the viral illness and affects everyone differently.
How common is long COVID?
Recovery from COVID-19 varies from person to person. Most people improve within a few days of the initial symptoms and recover within the first 4 weeks. For some it may take up to 12 weeks to fully recover, and for others, symptoms persist for much longer.
The severity of your case of COVID-19 doesn’t reflect your chances of developing symptoms of long COVID, how significant the persisting symptoms will be, or how long your symptoms will last.
What are the symptoms of long COVID?
Long COVID symptoms vary significantly as the illness can affect any system of the body. It can result in localised or multisystem inflammation, leading to abnormal functioning of various organs, as well as blood-clotting issues.
Common symptoms of long COVID include:
- fatigue
- fever
- aches/pains
- headache
- breathlessness and cough
- chest pain/tightness
- heart palpitations
- poor concentration or memory
- disrupted sleep
- dizziness
- pins and needles or numbness in the hands/feet
- abdominal pain, nausea and diarrhoea
- joint or muscle pains and weakness
- skin rashes
- earache and tinnitus
- loss of taste and/or smell
- sore throat
- low mood, anxiety and depression.
Note that the long-term psychosocial effect of COVID-19 can impact anyone, whether they’ve had the acute illness or not. You may have experienced the economic, financial and social impact of the pandemic, for example through loss of work, uncertainty of the future, and loss of social support systems – all of which can have an effect on your physical and emotional wellbeing.
How can I self-manage long COVID?
There are many things you can add to your daily routine to help manage some of the most common symptoms of long COVID.
Breathlessness
- Try breathing exercises: Focusing on your breathing, slowly take a deep breath in through your nose and then slowly breathe out through your mouth – putting a hand on your chest and stomach can help you concentrate on the movement as you breathe. Doing this for 5 minutes, several times a day, will help you control the rate and improve the depth of your breathing.
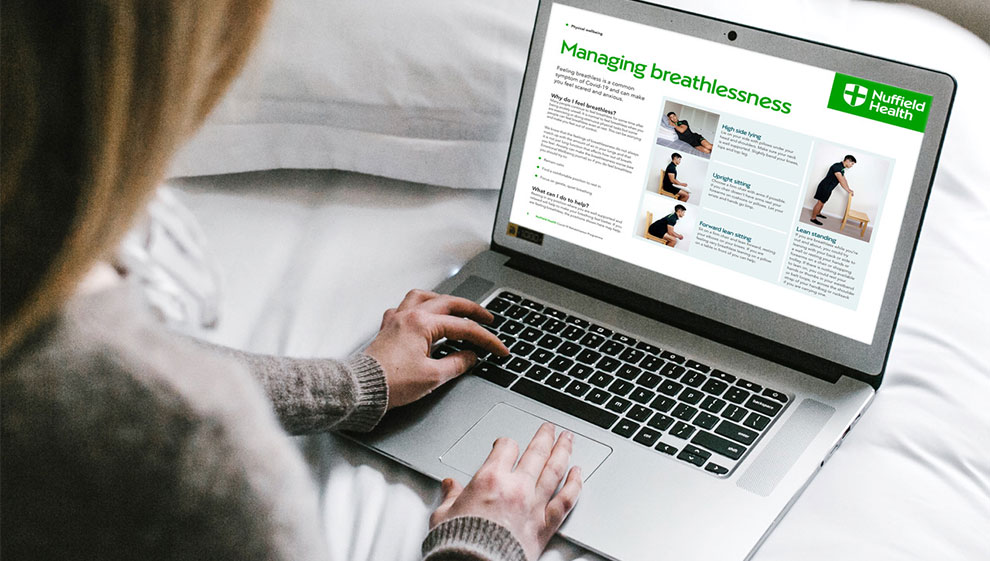
- Sit, lie or stand in certain positions: You can help ease breathlessness by either leaning forward while sitting and resting your hands on your lap; lying down with your knees bent and your feet flat on the floor; or standing up straight or leaning forward with the support of a stable surface.
- Gradually increase your daily exercise: If you can say a complete sentence without feeling breathless, then you can exercise harder. If you can’t speak at all, then you’re exercising too hard and should stop until your breathing has returned to normal. If you can complete a sentence, stopping twice to catch your breath, then you’re exercising at the right intensity.
Fatigue
- Go slow: Pace yourself and take regular breaks throughout the day.
- Plan your day around your energy levels: Do harder tasks at a time of the day when your energy levels are higher and break tasks down into smaller, more manageable, activities.
- Gradually increase your daily exercise: Listen to your body if you’re feeling tired and don’t push yourself.
- A–Z multivitamin supplements: These can help improve energy levels as well as maintain the health of your immune system.
Joint pain and muscle weakness
- Start with gentle exercises: Build yourself up slowly and stop if you're in any pain.
- Cardio exercises: Walking or climbing stairs will increase your energy levels, improve your breathing and lift your mood.
- Strength exercises: Lifting light weights or using resistance bands will keep your muscles strong and supple.
- Mobility exercises: Practising yoga or Pilates will keep your joints moving, while improving your balance and coordination.
- Vitamin D supplements: These can help maintain strong bones.
Poor concentration and memory
- Make a list of things you need to do for the day: Whether work-related or personal, this will help you plan your day and make tasks more manageable.
- Take regular short breaks throughout the day: Maybe set an alarm on your phone to remind you.
- Try to focus on one thing at a time: You may normally be able to multitask well, but when your memory and concentration are poor, focusing on one task at once is less distracting.
Anxiety or low mood
- Exercise: This can help to improve your mood as you release endorphins that make you feel good.
- Use meditation and breathing exercises: These can help calm your mind, lower your blood pressure and slow your heart rate down.
- Keep to a routine throughout your day: Wake up on time, start your day with breakfast, find an hour in the day for yourself – such as for exercise or meditation – unwind for an hour before you sleep, and go to bed at a reasonable time.
- Stay in touch with your family and friends: Socialising can help to lift the mood.
The Chartered Society of Physiotherapy also have a helpful website to self-manage low-grade symptoms – Covid-19: The Road to Recovery – while the World Health Organisation have put together a leaflet: Support for Rehabilitation Self-Management after COVID-19 Related Illness.
What options are there for long COVID rehabilitation?
In response to the increased demand for rehabilitation services, we launched our flagship COVID-19 Rehabilitation Programme in September 2020.
This sits alongside the NHS’s Your COVID Recovery online service and their Long COVID Centres across the UK.
Differences between these rehabilitation programmes
There is a wide spectrum of needs for people following a COVID-19 illness and it’s important to access the right rehabilitation at the right time:
- NHS Long COVID Centres – these provide face-to-face management for people with complex and severe symptoms who are in need of intensive rehabilitation and care
- NHS Your COVID Recovery online service – this 12-week online self-management programme is for people with low-level needs
- Nuffield Health’s COVID-19 Rehabilitation Programme – our programme provides rehabilitation to those between the two spectrums identified by the NHS Long COVID services and offers a combination of online access and face-to-face management over 12 weeks.
How to sign up for the programmes
You can be referred into any of the 3 rehabilitation programmes via GP (NHS or private), Community Care Professionals or Acute Hospital Clinics. You can self-refer into our COVID-19 Rehabilitation Programme, or into the NHS Your COVID Recovery online service.
Access to these programmes is free for anyone who has had confirmed or suspected COVID-19 and is continuing to suffer with symptoms beyond 4 weeks of the initial illness.
When to seek medical advice
If you’ve had suspected or confirmed COVID-19 and have persisting symptoms beyond 4 weeks of the initial infection, you should seek medical advice for a comprehensive assessment.
Last updated Friday 27 January 2023
First published on Monday 27 September 2021

