Hip replacement at Hereford Hospital
- Overview
Hip replacement, also known as total hip replacement (THR) or hip arthroplasty, is a surgical procedure to remove a damaged hip joint and replace it with an artificial joint (prosthesis) made of plastic, metal or ceramic. At Nuffield Health Hereford Hospital, our highly skilled orthopaedic consultants take a personalised approach to your hip replacement, helping you to return to the activities you love.
The hip joint
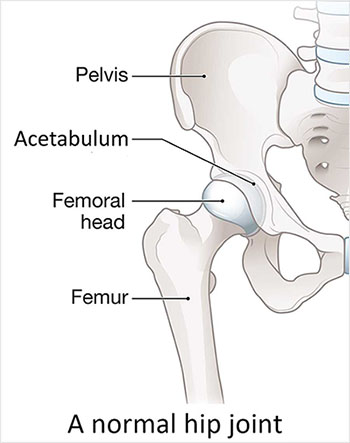
The hip is a ball-and-socket joint, where the rounded head of the femur (thighbone) is the “ball” and fits into the acetabulum (the “socket” in the pelvis).
Both the ball and socket are normally covered in smooth tissue called articular cartilage. The cartilage cushions the bones, allowing for easy, almost friction-free movement, such as walking and bending.
A hip replacement becomes necessary when the cartilage in the hip joint becomes worn or damaged, resulting in pain, stiffness and reduced movement. This often makes everyday activities such as walking, standing and climbing stairs difficult.
What can cause damage to the hip joint?
Several conditions can lead to the need for hip replacement surgery:
- Osteoarthritis: Often called “wear and tear” arthritis, the cartilage gradually wears away, causing the bones to rub against each other. This causes hip or groin pain, swelling, stiffness and reduced movement. This is the most common reason for hip replacement, especially in older adults.
- Rheumatoid arthritis: This is an autoimmune disease where the body's immune system mistakenly attacks the lining of the joint (synovium). This causes chronic inflammation, pain, swelling, and over time, damages the cartilage and bone.
- Post-traumatic arthritis: This type of arthritis can develop after an injury to the hip, such as a fracture or dislocation. The injury permanently damages the cartilage, which leads to arthritis years later.
- Hip fracture: Some hip fractures are best treated with a partial or total hip replacement. This is more likely if the fracture has damaged the blood supply to the head of the femur, or if the bone is severely broken or unlikely to heal with fixation alone.
- Childhood disorders such as hip dysplasia (a poorly formed hip socket) or Perthes disease (a temporary loss of blood supply to the femoral head in childhood) lead to joint damage and arthritis. As a result, patients may need a hip replacement much earlier than usual, typically in their 40s or 50s.
Do I need a hip replacement?
Your consultant may recommend hip replacement surgery if:
- You have tried non-surgical options such as physiotherapy, walking aids, pain relief medicine and joint injections, but they have not improved your symptoms.
- You have ongoing hip or groin pain that significantly affects your daily life, making it difficult to walk, exercise or do everyday activities.
- Your hip pain is severe enough to keep you awake at night or stop you from falling asleep.
- You have stiffness in your hip and your range of movement is reduced, making daily tasks such as climbing stairs, getting in or out of a chair, or putting on shoes/socks very difficult.
If you're experiencing severe symptoms in both hip joints, your consultant may discuss a bilateral hip replacement with you. This means replacing both hip joints during a single operation (simultaneously) or in two separate surgeries (staged).
Over 90,000 people have hip replacement surgery each year in the UK1, and for most, it brings less pain, better movement and a noticeable improvement in day-to-day quality of life.
Why choose Nuffield Health Hereford Hospital for your hip replacement surgery?
Just a short distance from Hereford city centre, Hereford Hospital provides exceptional private healthcare for you. Our experienced orthopaedic surgeons and matron-led nursing teams will give you care that's tailored to you.
To ensure a peaceful recovery, you will stay in a modern, private en-suite room designed for maximum comfort. Each room is a clean, contemporary space fully equipped with a flatscreen TV and complimentary WiFi, allowing you to recover in a relaxing environment that feels more like home than a hospital.
How to book a consultation at Nuffield Health Hereford Hospital
If you're suffering from hip pain and think you're suitable for hip replacement surgery, you can arrange a private consultation with one of our expert orthopaedic surgeons today by booking an appointment online, calling 01432 687 029 or by filling in the form below.
How long does a hip replacement last?
Hip replacements can last a long time - around 15 to 20 years, depending on your age, activity level, general health and the type of implant you have. Your consultant will discuss the best implant option for you.
However, when a hip implant does need to be replaced, you will need to have a hip revision.
What happens during hip replacement surgery at Nuffield Health Hereford Hospital?
Hip replacement surgery usually takes around 60 to 90 minutes. It’s preferably done under spinal anaesthetic, which numbs the lower half of your body. You may also be given a sedative to relax you, or if you prefer to be unaware of noises and activity during the surgery.
If spinal anaesthetic is not appropriate, the other option is general anaesthetic, which sends you to sleep. Your consultant or anaesthetist will discuss your options with you.
Preparing for surgery
There are a few things you can do in the weeks leading up to your surgery to help everything go as smoothly as possible and support your recovery:
- Stay as active as you can: Gentle exercises such as walking, yoga, Pilates and swimming can help to improve your range of movement which will help your recovery. While surgery will relieve the pain caused by arthritis, it cannot automatically restore a lost range of motion. To increase your range of motion after surgery, you should follow an exercise plan and physiotherapy to gently stretch the tight muscles and tendons surrounding the hip.
- Physiotherapy or prehabilitation: Working with a physiotherapist before your surgery can help you to strengthen the muscles and, more importantly, improve your range of motion. At Nuffield Health, we offer pre-operative physiotherapy sessions for all hip replacement patients. These sessions will help you prepare your body, improve your movement, and set the stage for a smoother recovery after surgery.
- Stop smoking or vaping: If you smoke or vape, stop several weeks before the operation, as nicotine can affect wound healing.
- Try to maintain a healthy weight: A healthy weight can reduce the strain on your new hip.
- Prepare your home for recovery: A thorough assessment of your home is often recommended, especially for older patients or those who live alone. Remove trip hazards such as loose rugs and move items you use frequently within easy reach. You will likely need a raised toilet seat, a shower bench and grab bars. If you have stairs, it might be necessary to stay on a single floor of your home for a short time after the operation.
- Arrange transportation: You won't be able to drive after surgery, so make sure someone can pick you up from the hospital and take you home.
- Arrange support: Ask family and friends to help with essential tasks like driving, cooking and shopping for the first few weeks after you return home.
Find out more about preparing for surgery.
Before the surgery
You will have a pre-assessment appointment before your hip replacement with your consultant and healthcare team.
They will review your medical history and may ask you to complete some diagnostic tests, such as X-rays and blood tests.
Be sure to:
- Let your doctor know about any medication you take. They will let you know if you should continue or temporarily stop any medicines before and after your surgery.
- Let your doctor and healthcare team know about any conditions you have such as diabetes and high blood pressure.
Follow any instructions for fasting before your surgery (usually no food or drink for several hours before your surgery).
Find out more about the pre-assessment appointment.
During the procedure
- Once you’re under anaesthetic, your surgeon will cut the hip joint. Depending on the surgical technique, the cut may be on the front, side, or back of your hip.
- Your surgeon will carefully move the muscles and tissues aside to expose the hip joint.
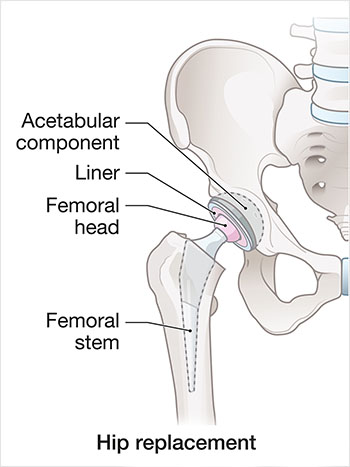
- The femoral head (the “ball” at the top of the thigh bone) is dislocated from the acetabulum (the “socket” in the pelvis) and then surgically removed.
- The damaged cartilage and bone are removed from the hip socket. The socket is carefully shaped and a new socket (acetabular cup) is inserted.
- The femur (thighbone) is prepared and a metal stem (femoral stem) is inserted and fixed into place with cement or a special coating that will bond it directly to the bone.
- The new artificial ball (femoral head) is attached to the top of the metal stem.
- At this point, the surgeon will have created a stable ball-and-socket hip joint.
- Finally, the wound is closed with stitches or surgical clips. A sterile dressing is applied to the wound. Some stitches are dissolvable, but clips will always need to be removed.
If you are having a simultaneous bilateral hip replacement, the surgeon repeats the replacement process for the second hip joint immediately after the first.
After the surgery
You’ll be taken to the recovery area until you are awake and stable. A nurse will be at your side when you wake up and stay with you throughout your recovery.
You may have a drip (infusion) going into your arm to keep you hydrated and give you pain relief.
When the nurse and anaesthetist are happy with your recovery, you will be taken to your room.
Recovery from hip replacement
Recovery from hip replacement surgery may take up to 8 weeks, depending on your age and general health. However, improvements can be noticeable for up to 12 months.
Recovery at the hospital
You will stay in the hospital for one to two nights. You will be given painkillers to help manage your pain.
To prevent blood clots, you may be given blood-thinning medicine, wear compression socks, or have pneumatic compression devices on your legs.
You will be encouraged to start walking as soon as possible, usually on the same day as your operation or the day after.
A physiotherapist helps teach you how to walk using a walking frame or crutches. They will also teach how to get in and out of a bed, a chair and a toilet, and use stairs. They will show you exercises to do in the hospital and at home to help with your recovery.
You’ll be able to go home as soon as you can manage stairs safely, walk safely with crutches or a walking aid, and your healthcare team are happy with your recovery. You won’t be able to drive, so please arrange for someone to take you home.
Recovery at home
You may feel quite tired when you get home, so get plenty of rest. Then it’s important to slowly increase your activity.
You will have been advised of your hip precautions by your consultant and healthcare team before the surgery.
There are a few things you can do at home to help strengthen your hip, avoid damaging it and help your wound heal:
- Staying as mobile as possible will help reduce the risk of blood clots and quickly bring down swelling and bruising.
- Make sure to do the exercises the physiotherapist showed you 3 or 4 times a day, for at least 6 weeks.
- Gradually increase how far you walk.
- Don’t lift anything heavy or do any strenuous exercise.
- Avoid twisting your hip when standing.
- Take a shower instead of a bath.
- Avoid sitting on excessively low sofas and chairs.
- You may be required to sleep on your back for a few weeks.
Physiotherapy is an essential part of hip replacement recovery because increasing your range of movement and building up strength in the muscles around your new joint will help you get back to your normal activities.
After your hip replacement surgery, your physiotherapist will give you clear advice on what you can and cannot do and guide you towards restoring your mobility and confidence.
Pain after hip replacement surgery
Pain can be managed with pain relief medicine given by hospital staff or prescribed by your consultant.
Pain will decrease significantly and be managed with prescribed pain relief medicine.
Pain can be managed with over-the-counter painkillers.
Most patients do not need pain relief at this stage.
Pain doesn’t interfere with daily tasks, but you might feel sore after exercise or a long walk.
You should not need any pain relief.
What are the risks and complications of a hip replacement?
Most people recover well from a hip replacement, but like any surgery, it carries risks — from general complications to those specific to hip replacement surgery. Your consultant (surgeon) will talk you through these risks, answer any questions and help you feel more confident going into surgery.
General complications may include:
- Bleeding: Some bleeding is expected during and after surgery, but bleeding after you have been discharged from the hospital should be reported to your consultant.
- Infection of the surgical site (wound): Let your consultant or healthcare team know any concerns about infection at the earliest opportunity. Seek their guidance first before going to your GP.
- Allergies: Let your consultant and healthcare team know if you have any allergies or have reacted to any medicine, tests or dressings in the past.
- Blood clots (Deep vein Thrombosis DVT): A risk associated with any surgery.
Specific complications of hip replacement surgery:
- Nerve damage: Injury to the nerves around your hip, leading to weakness, numbness or pain in your leg or foot.
- Blood vessel damage: Damage to blood vessels around your hip, leading to loss of circulation to your leg and foot.
- Fracture: If the bone is weak, it may split when the femoral stem is inserted.
- Leg length difference: Your surgeon will try and make sure your legs are the same length, but this is not always possible.
- Infection: An infection in your hip can cause the implant to loosen or fail.
- Dislocation: Although rare, you may require another surgery if it keeps happening.
- Heterotopic ossification: Bone forming in muscles around your hip replacement.
- Difficulty passing urine: You may require a catheter after surgery and although this is rare. Difficulty passing urine is more common in people with certain underlying conditions, e.g. enlarged prostates.
How much does hip replacement surgery cost at Nuffield Health Hereford Hospital?
Please note that the guide price stated is an approximate cost of treatment only. You will be given a fixed all-inclusive price for treatment following your initial consultation with a consultant.
FAQs
-
Is hip replacement a major surgery?Yes, total hip replacement is a routine surgery , but also major due to the complexity of the procedure (the removal of the natural hip joint and the insertion of a large implant) and the length of recovery (up to 12 months).
-
Will an X-ray show if I need a hip replacement?An X-ray is an important test because it shows how badly damaged the hip joint is. However, an X-ray alone cannot confirm if you need hip replacement surgery.
Your consultant will also consider your symptoms (e.g. pain, stiffness, reduction in mobility) before deciding if you are suitable for a hip replacement. -
Which method of hip replacement is the best?There is no single “best” method. The most effective approach for you depends on your anatomy, your condition and your surgeon’s expertise.
There main difference is the surgical approach (where the cut is made):- Posterior approach: Back of the hip (buttock)
- Anterior approach: Front of the hip (groin area)
- Lateral approach: Side of the hip
-
Can I get both hips replaced at the same time?If you have severe arthritis in both hips, you can get both hip joints replaced - known as a bilateral hip replacement. This can be performed in one operation (simultaneous bilateral hip replacement) or in two seperate operations (staged bilateral hip replacement). Your consultant will review your medical history and physical fitness to recommend the safest path for your recovery.
-
How long does a hip replacement take?Hip replacement surgery takes between 60 to 90 minutes.
-
How long will I stay in the hospital after hip replacement?You will stay in hospital for 1 to 2 nights. However, you will not be discharged until you can walk up and down stairs, with a walking aid, and your healthcare team are happy with your recovery.
-
Will I have scars after hip replacement?Yes, you will have a scar where the cut (incision) was made. The scar maybe on the side, back or front of the hip, depending on the surgical technique used. It is usually 10 to 20cm long.
The scar may appear raised and red soon after surgery, but it will flatten and the colour will fade as you heal. -
How far can I walk two weeks after surgery?There is no exact distance anyone should be able to walk two weeks after surgery.
You should focus on walking frequently (for short periods) and doing your physiotherapy exercises. -
How long after hip replacement surgery can I drive?You can start driving around 4 to 6 weeks after a hip replacement, depending on which leg was operated on.
You must be able to get safely in and out of the car, control the pedals confidently and perform an emergency stop without hesitation or severe pain. -
What can I never do after hip replacement?There are a few things you must avoid after hip replacement surgery:
- High-impact sports and contact sports should be avoided. Sports such as basketball, volleyball, aerobics and football, should be discussed with your surgeon.
- Deep squatting with heavy weights.
-
When can I use a regular toilet after hip replacement surgery?You must use a raised toilet seat for at least six weeks. The low height of a standard toilet seat may increase the risk of dislocation (where the joint pops out of the socket).
At your follow-up appointment, your consultant or physiotherapist will check how you’re healing and let you know if it’s safe to go back to a normal height toilet seat. -
When can I sit on sofa after hip replacement?You should avoid excessively low sofas and chairs for at least 6 weeks after your hip replacement. Sitting on a low or soft surface increases the risk of dislocation (where the joint pops out of the socket).
You should sit on high, firm chairs with armrests. Armrests allow you to safely push yourself up without up without twisting or bending your hip. -
How soon can I fly after hip replacement?You should avoid flying long-haul for 12 weeks after your hip replacement as the risk of blood clots in the legs (DVT) is higher.
If you need to fly, please discuss this with your consultant. They may recommend taking blood thinners, wearing compression socks and walk the aisle every hour. -
When can I wear jeans after hip replacement?You can start wearing jeans after the swelling has gone down and you can bend your hip comfortably to get them on and off. As soon as you feel comfortable to, you can.
Sources
1 - The National Joint Registry 17th Annual Report 2020
Hip replacement consultants at Hereford Hospital
Venns Lane, Hereford, HR1 1DF
Guide price
| Initial consultation | from £150 | |
|---|---|---|
| Diagnostics | If needed to determine treatment plan | |
| Treatment | £16,325 | |
| Pre-assessment | Included | |
| Main treatment | Included | |
| Post-discharge care | Included | |
| Pre-assessment, Main treatment and Post-discharge care | £16,325 | |
| Guide price | £16,475 | |
The guide price
stated above is an approximation of the cost of treatment only. The final price
may vary according to Consultant fees, prosthesis or drugs used and any
pre-existing medical conditions which may alter your care pathway.
You will be given a fixed all-inclusive price for treatment following
your initial consultation with a Consultant.
Ways to pay
Nuffield Health promise
Our prices are all-inclusive. We will equal any comparable price. There are no time limits on your aftercare.
Paying for yourself
There are no hidden costs in our treatment prices. The price you see is the price you pay.
Find out morePersonal medical loan
Spread the cost of your treatment with a 10, 12 or 24 month 0% personal medical loan.
Find out moreMedical insurance
We work with you and your insurance provider to get you the treatment you need quickly
Find out more